Knowledge base » Visit forms » Cancer Assessment & History Form
Cancer Assessment & History Form
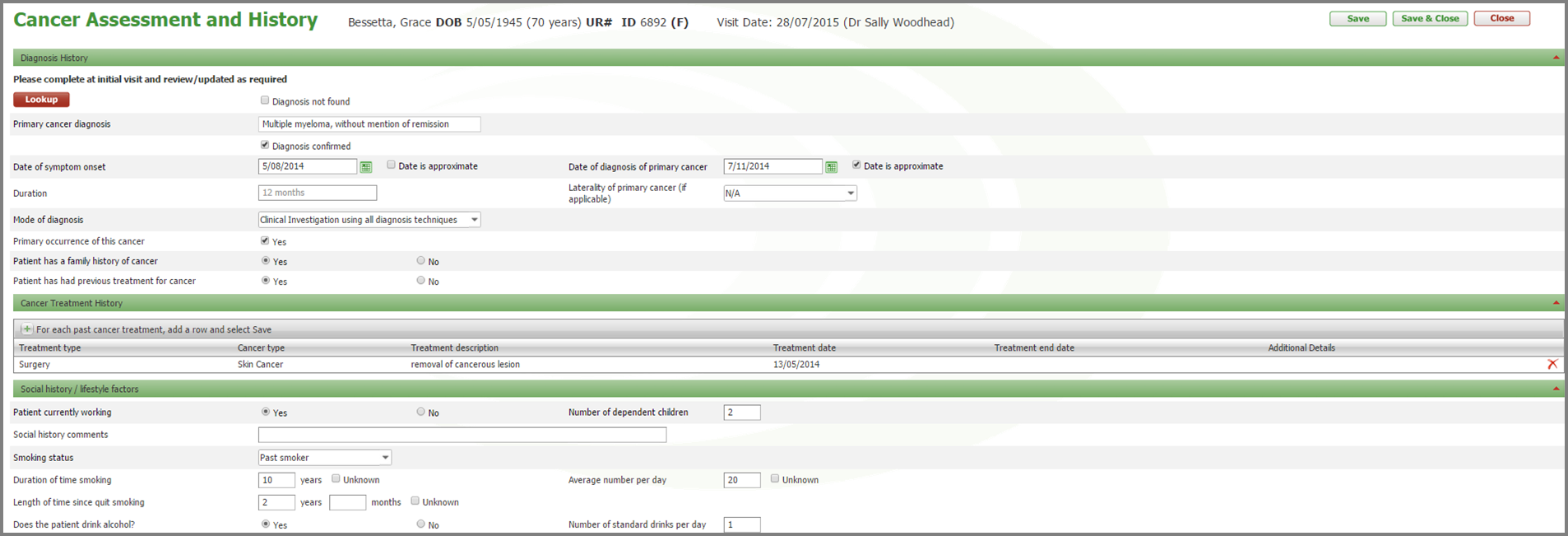
This form is used to record the patients primary diagnosis (which is copied to the conditions & allergies form). Duration of disease, date of diagnosis, method of diagnosis. Family history and personal history of cancer.
If the patient has had previous cancer treatment cancer treatment history grid will appear where details of previous treatment can be recorded.
The following section is where social and lifestyle factors are recorded.
For patients that have or currently smoke there are a number of smoking questions.
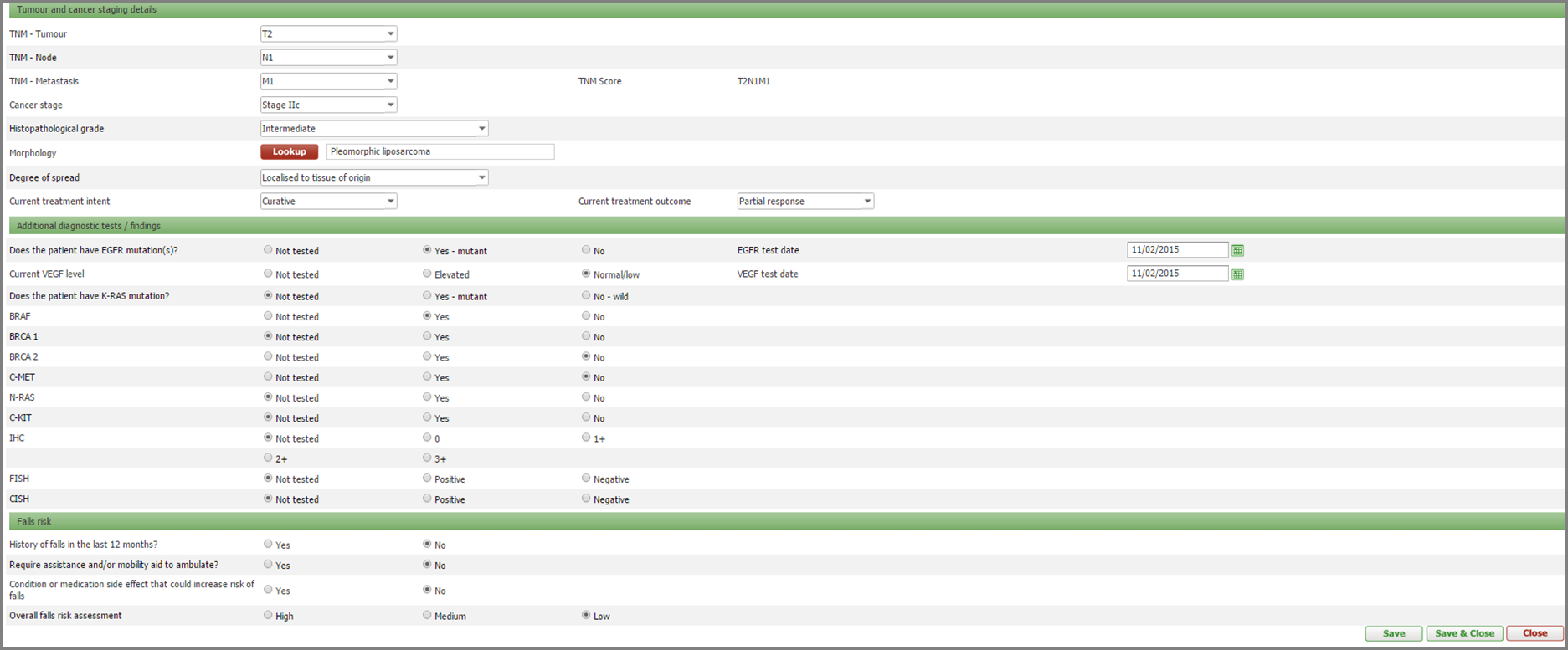
The second half of the history form is where TNM score is calculated, morphology, spread, treatment intent, genetic testing and falls risk are recorded. The page dynamically renders additional questions if the visit reason is breast or prostate cancer.
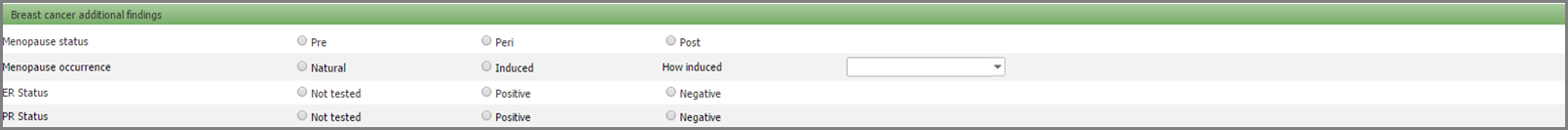
If the visit reason is breast cancer the following additional questions appear on the form.
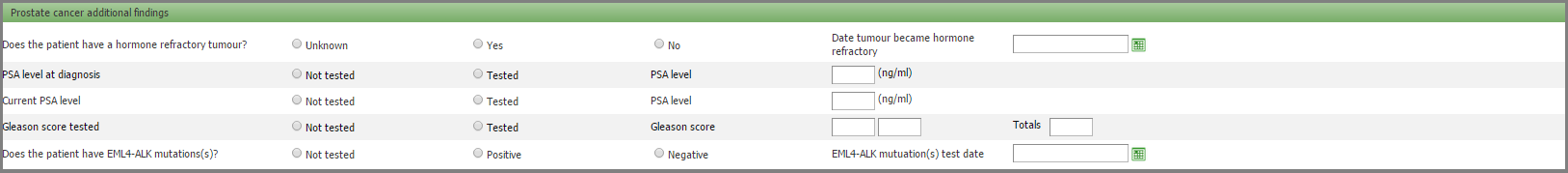
If the visit reason is prostate cancer the following additional questions appear on the form.
If the patient has had previous cancer treatment cancer treatment history grid will appear where details of previous treatment can be recorded.
The following section is where social and lifestyle factors are recorded.
For patients that have or currently smoke there are a number of smoking questions.
The second half of the history form is where TNM score is calculated, morphology, spread, treatment intent, genetic testing and falls risk are recorded. The page dynamically renders additional questions if the visit reason is breast or prostate cancer.
If the visit reason is breast cancer the following additional questions appear on the form.
If the visit reason is prostate cancer the following additional questions appear on the form.


